Discover a brief account of medical gaslighting and chronic pain dismissal in a defiant cry for self-advocacy.
Table of Contents
Humiliation that burns as hot as the nerve pain in my arms? Wasn’t quite what I was expecting to receive at the hospital. Yesterday, I walked into the pain clinic with the slim hope of finding relief. I was already skeptical of the answers I could seek for my chronic pain under the cracks in universal healthcare. But I still wasn’t prepared to leave so disheartened and dismissed.
My doctor isn’t a cardboard cutout of a villain. He is someone I have went to for years, and one of the most seemingly empathetic figures in the local healthcare scene. (Although this isn’t saying a lot.) Yet he told me point blank that my chronic pain is “in my head.” Not that my brain is misfiring signals—an explanation I can rationally understand—but that my pain stems entirely from psychological issues.
I’m here to tell you why this is wrong—not just morally, but also logically.
How My Doctor Dismissed My Chronic Pain
My doctor dismissed my medical history. I find this to be a dangerous overstep, where my health and potentially life are what’s at stake. Why am I confident in saying this? Because I have prior experiences where similar claims were made but proven wrong. For example:
• From 2017-2019 was told that my throat was closing up due to panic attacks. It turned out I needed emergency sinus surgery to remove an almost 100% obstructed passageway. I spent two years having my throat close, with only epi pens opening it up. (I was told at the time it was psychosomatic that the pens worked.)
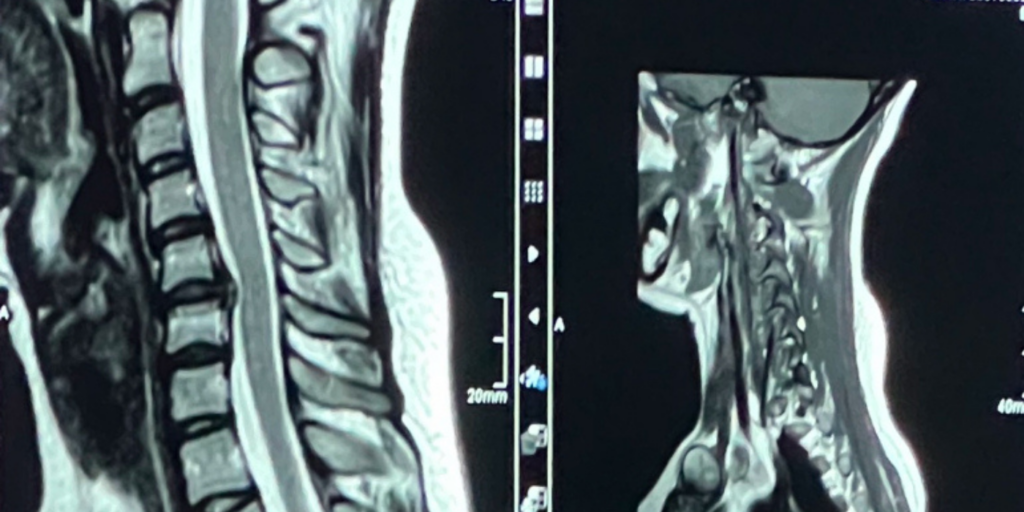
• My neck and upper back pain was attributed to “stress,” but imaging I pursed for years and paid thousands of dollars out of pocket for revealed spinal degeneration that required urgent surgery held days before Christmas in 2023.
Both times, I was labeled as “emotional” or a “hypochondriac.” Both times, the underlying issues were real.
Yet, despite this track record of self-advocacy and accurate instincts about my body, my pain clinic doctor dismissed me again. He claimed I was the type of patient who “always demands more,” who “wants unnecessary surgeries,” and who will “never be happy.” He accused me of being like the “difficult patients” who make things worse for themselves.
I paraphrase these words immediately after the event, though I can assure you of the accuracy of the statements, as my boyfriend bore witness. In fact, here is a message I sent him while we were still at the appointment.
This isn’t just hurtful — it’s harmful, and it’s a clear example of medical gaslighting.
Why Dismissing Chronic Pain is Wrong
1. Dismissing Real Pain as Psychological: Chronic pain is complex and multifaceted, often requiring a combination of physical, medical, and psychological treatments. Suggesting my pain is entirely “mental” ignores the reality of my medical history and invalidates my lived experience.
2. Unwarranted Bias: The doctor categorized me as a “difficult patient” based on his own biases rather than evidence. Chronic pain patients—especially women—are often unfairly labeled as “hysterical,” “attention-seeking,” or “demanding.” This bias leads to missed diagnoses and untreated conditions. Medical gaslighting is not just frustrating—it’s dangerous.
3. Failure to Collaborate: Instead of exploring all possible treatment options, the doctor shut down my concerns and refused to legitimately explore the alternatives I know exist. His refusal to engage in shared decision-making is a failure of care.
Though he reviewed the options I presented due to research I only did when no one told me I had options, I was not told I couldn’t receive any advanced care except for perhaps a different medication—and paperwork for therapy. (By the way, the therapy intake papers at the hospital asked if I ever had homosexual thoughts … a very safe option for a queer woman to receive therapy.)
4. Dismissive and Dehumanizing Language: Comparing me to “difficult patients” and accusing me of hypochondria is not only unprofessional but also damaging. It perpetuates stigma, makes patients feel unheard, and discourages them from seeking further help.
I was also told I was like a character in “House of God,” someone who receives all of the antidepressants in the world and is not happy. I assume this was a dig because I take antidepressants. However, I am happy with my mental health and was not complaining about it. Therefore, I found this comment to be out of line.
Why I Deserve to Advocate for Myself—And So Do You
I won’t lie, for a few minutes I really doubted myself and questioned if I deserve anything. The humiliation burned deep and hot, but so did the pain in my body. This wasn’t light pain; it was the kind of pain I could not ignore. Despite it, I hold a full-time job, a relationship, friendships, and plenty of hobbies. I pursue a passionate and fulfilling life. I know I’m not inventing issues because I am bored.
I’ve proven time and time again that my instincts about my body are correct. I don’t seek unnecessary treatments; I seek necessary ones to prevent further harm and improve my quality of life. My spine surgery wasn’t about expecting a miraculous cure—it was about addressing a bulging disc that would have worsened over time. My pain is not a desire for attention; it’s a call for help.
Doctors don’t live with my pain. They don’t feel the burning nerve pain that makes daily life at times close to unbearable. They don’t carry the weight of being dismissed or the frustration of fighting for answers. But I do. And that’s why I won’t stop advocating for myself.
I’ve already contacted specialists at top clinics, including the neuro department at a university hospital in Cologne. The chief of the department personally responded and offered to review my case. This gives me hope that someone will take me seriously, listen to my story, and work with me to find solutions for chronic pain help.
Closing Words: Bias Against Women in Medicine
Unfortunately, my experience is not unique. Studies show that women’s pain is often dismissed or minimized in healthcare settings. Chronic pain patients, in particular, are labeled as “difficult” or “overly emotional.” This bias against women in medicine can delay diagnosis, limit treatment options, and lead to further physical and emotional suffering.
This is why speaking up matters. By sharing my story, I hope to shed light on the biases that plague chronic pain care. Pain—physical or emotional—is never something you should just “accept” without exploring every reasonable avenue for improvement, especially when seeking chronic pain help.
And please, doctors who dismiss cases as hysteria, try to view things more logically and a bit less emotionally next time.
Continued Reading: Medical Gaslighting & Healthcare Stigmatization
